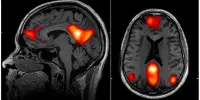
There is mounting evidence that certain infections can impair cognitive performance in middle-aged and older adults. A new study discovered that symptoms of common infections were associated with poorer performance on a test of global cognitive function in a sample of middle-aged and older adults.
A new study led by Johns Hopkins Bloomberg School of Public Health researchers discovered that signs of common infections in a sample of middle-aged and older adults were associated with lower performance on a test of global cognitive function. The findings add to a growing body of evidence that infections in middle and late life can impair cognitive function and increase the risk of Alzheimer’s disease and other dementias.
The researchers examined antibody levels to five common pathogens in 575 adults ranging in age from 41 to 97. The adults were recruited from East Baltimore in 1981 as part of the National Institute of Mental Health’s Epidemiologic Catchment Area Study, which began that year.
The idea that common infections could contribute to cognitive decline and perhaps Alzheimer’s disease risk was once on the fringe and remains controversial, but due to findings like the ones from this study, it’s starting to get more mainstream attention.
Adam Spira
During the same study period, participants in the Baltimore study donated blood for testing and took cognitive tests. Antibody tests for pathogens such as herpes simplex virus type 1, cytomegalovirus, varicella zoster virus (chickenpox and shingles viruses), and Epstein-Barr virus, as well as the parasite Toxoplasma gondii, were performed. The latter is frequently transmitted to humans through cat feces or by eating raw meat.
The researchers compared the results of the blood tests to the participants’ performance on the Mini-Mental State Examination (a global cognitive test that assesses things like orientation, attention, verbal comprehension, memory, and visual perception) and a word recall task, which tested memory for a list of words after a 20-minute delay. The researchers discovered that elevated antibodies to herpes simplex virus type 1 or cytomegalovirus were each associated with poor performance on the global cognitive test. Furthermore, participants who had a greater number of positive antibody tests missed a greater number of items on the global cognition test.
The study was published in the journal Alzheimer’s & Dementia online.

“The idea that common infections could contribute to cognitive decline and perhaps Alzheimer’s disease risk was once on the fringe and remains controversial, but due to findings like the ones from this study, it’s starting to get more mainstream attention,” says senior author Adam Spira, Ph.D., professor in the Bloomberg School’s Department of Mental Health and a core faculty member of the Johns Hopkins Center on Aging and Health.
“After accounting for participants’ age, sex, race, and the largest genetic risk factor for Alzheimer’s disease, the data in our study showed that a greater number of positive antibody tests related to five different infections was associated with poorer cognitive performance. To our knowledge, this kind of additive effect of multiple infections on performance on a cognitive test has not been shown before.”
The cause of Alzheimer’s disease is unknown. Prior research has linked infections to an increased risk of Alzheimer’s disease, including studies linking herpes simplex virus type 1 and cytomegalovirus. There is also evidence that the protein fragment amyloid beta, which forms insoluble plaques in Alzheimer’s patients’ brains, serves as an antimicrobial peptide and is secreted at higher levels by brain cells in response to infections.
Since the 2003-2004 wave, Johns Hopkins ECA study researchers have conducted periodic follow-up interviews in Baltimore, including standard cognitive tests and blood samples. The National Institute on Aging funded the two most recent waves of the study, which focused on Alzheimer’s disease and related outcomes.
The pathogens studied are frequently encountered in childhood and are either cleared or transformed into suppressed, latent infections. As a result, the researchers regarded significant levels of antibodies against them in the study’s middle-aged and older participants as likely indicators of reactivation due to immune system weakening with age.
Alexandra Wennberg, PhD, the study’s first author, completed her doctoral training in Spira’s research group and is now a postdoctoral research associate at Sweden’s Karolinska Institutet. Faculty from the Johns Hopkins School of Medicine are among the co-authors, as are scientists from the National Institute on Aging Intramural Research Program.